When it comes to battling metastatic colon cancer peritoneal cavity, the journey is filled with unique challenges, such as rapid progression, poor prognosis, and limited treatment options. Yet, the relentless pursuit of knowledge and advances in treatment techniques offer hope and improved outcomes. This comprehensive guide takes you through the complex landscape of metastatic colon cancer peritoneal cavity, from understanding the metastatic process to exploring the latest clinical trials and personalized approaches that can make a difference in patients’ lives.
Key Takeaways
-
Metastatic colon cancer in the peritoneal cavity is challenging to treat, but early detection improves survival rates.
-
Cytoreductive surgery (CRS), hyperthermic intraperitoneal chemotherapy (HIPEC) and systemic chemotherapy are main treatment options for metastatic colon cancer in the peritoneal cavity.
-
Clinical trials have led to new treatments such as HIPEC, PRODIGE-7 trial, PIPAC and immunotherapy. Prognostic factors also influence outcomes and quality of life can be improved through pain management, nutritional support & psychological support.
My Top 10 Learnings
Don’t miss our
free Guide
10 Things I Wish I Knew Before My Cancer Treatment
Metastatic Colon Cancer and Peritoneal Cavity
Peritoneal metastatic colorectal cancer is a complex disease to treat due to its swift advancement, unfavorable prognosis, and restricted treatment options. Historically, the outlook for patients with peritoneal carcinomatosis of colorectal origin has been unfavorable. As recent as the 1990s, median survival rates for patients with colorectal peritoneal metastasis were limited to just six months.
However, the treatment scenario has been evolving. Advances in surgery and hyperthermic intraperitoneal chemotherapy (HIPEC) treatments have improved the median overall survival from 6.0 months between 1995 and 2000 to 12.5 months between 2010 and 2014. Despite these advancements, the prognosis is still relatively poor compared to other cancer metastasis sites, underscoring the need for early detection and intervention.
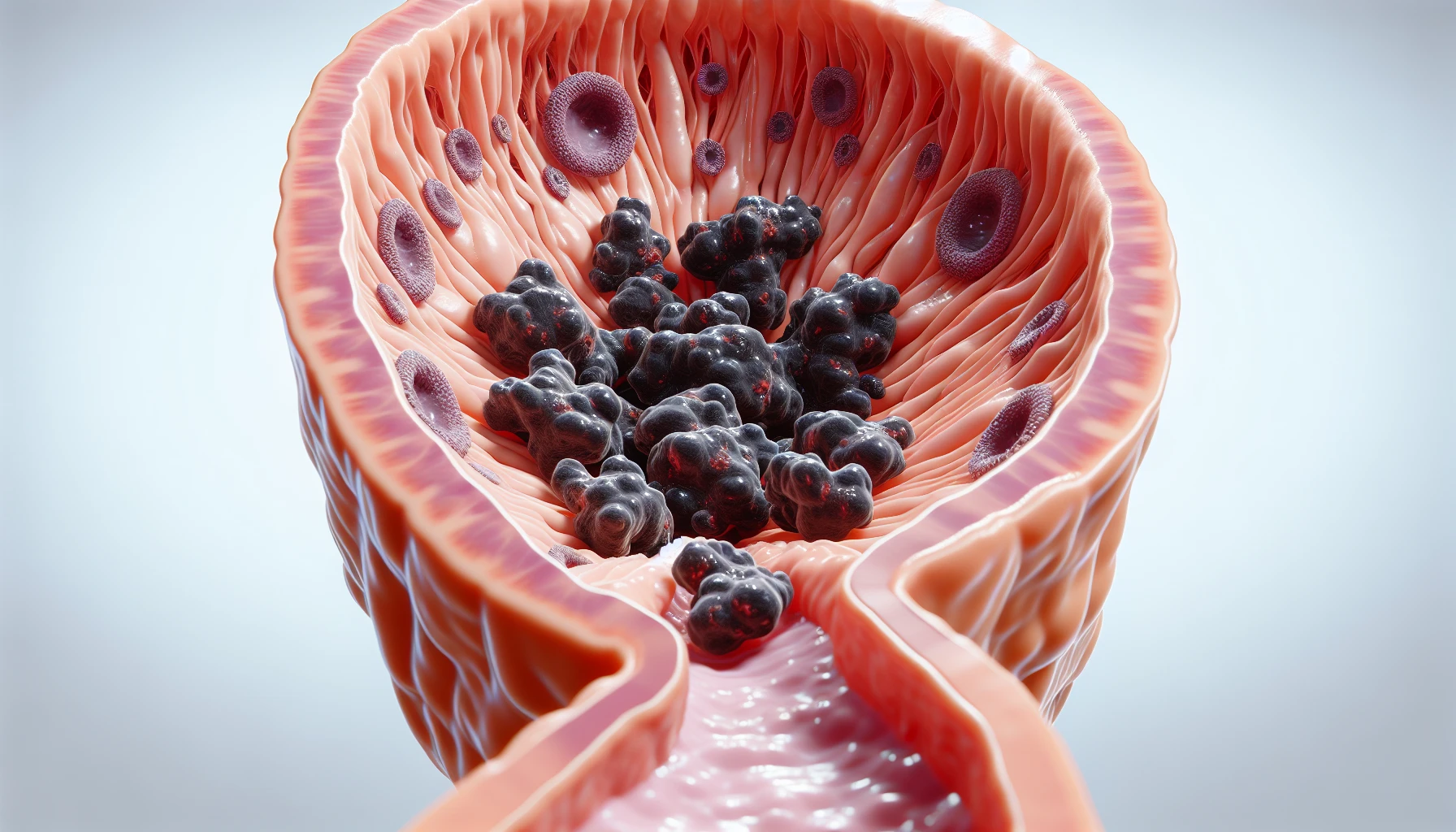
Metastatic Process and Peritoneal Cavity
The peritoneal cavity is a membrane-lined space within the abdomen that houses organs and other structures. Metastatic colon cancer cells leave the primary site and form new colonies in distant tissues, a process known as the invasion-metastasis cascade. The liver and lung are the two most common sites of metastasis for colorectal cancer patients. The peritoneal cavity follows, accounting for 11% of such cases. A lack of vascularization in the peritoneum results in peritoneal metastases spreading through the locoregional route, adding to the challenge of treating this condition.
While resection of liver metastasis in CRC patients remains the only treatment with curative intent, the development of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (HIPEC) has provided new hope for patients with peritoneal metastases. The key lies in detecting peritoneal metastasis early to enhance survival rates and treatment outcomes.
Challenges in Treating Peritoneal Metastases
Treating peritoneal metastases is filled with difficulties, mainly because of the condition’s low sensitivity to systemic therapy. Factors such as limited penetration of chemotherapy into the peritoneum and low tumor-targeting specificity contribute to the limited efficacy of systemic therapy in peritoneal metastases. Furthermore, peritoneal metastases have a higher systemic disease burden than other metastasis sites, complicating treatment and management.
Surgical approaches, such as CRS and HIPEC, have emerged as potential treatment options for peritoneal metastases. However, these procedures also come with potential complications, such as post-operative adhesions, distorted anatomy, and uncertain long-term survival impacts. Consequently, careful patient selection and personalized treatment approaches are crucial for optimizing outcomes in this challenging setting.
Importance of Early Detection
The significance of early detection is paramount. Diagnostic laparoscopy and advancements in radiological assessment and imaging techniques have enabled the early detection of peritoneal metastases from colon cancer. By identifying peritoneal metastases early, more effective treatment options can be employed, potentially improving survival rates and overall treatment outcomes for patients.
Treatment Options for Metastatic Colon Cancer in the Peritoneal Cavity
At present, the main treatment options for metastatic colon cancer in the peritoneal cavity consist of cytoreductive surgery (CRS), hyperthermic intraperitoneal chemotherapy (HIPEC), and systemic chemotherapy. Each of these treatment options has its own advantages and disadvantages, and their effectiveness can be influenced by various factors, such as patient selection, tumor characteristics, and the extent of peritoneal disease.
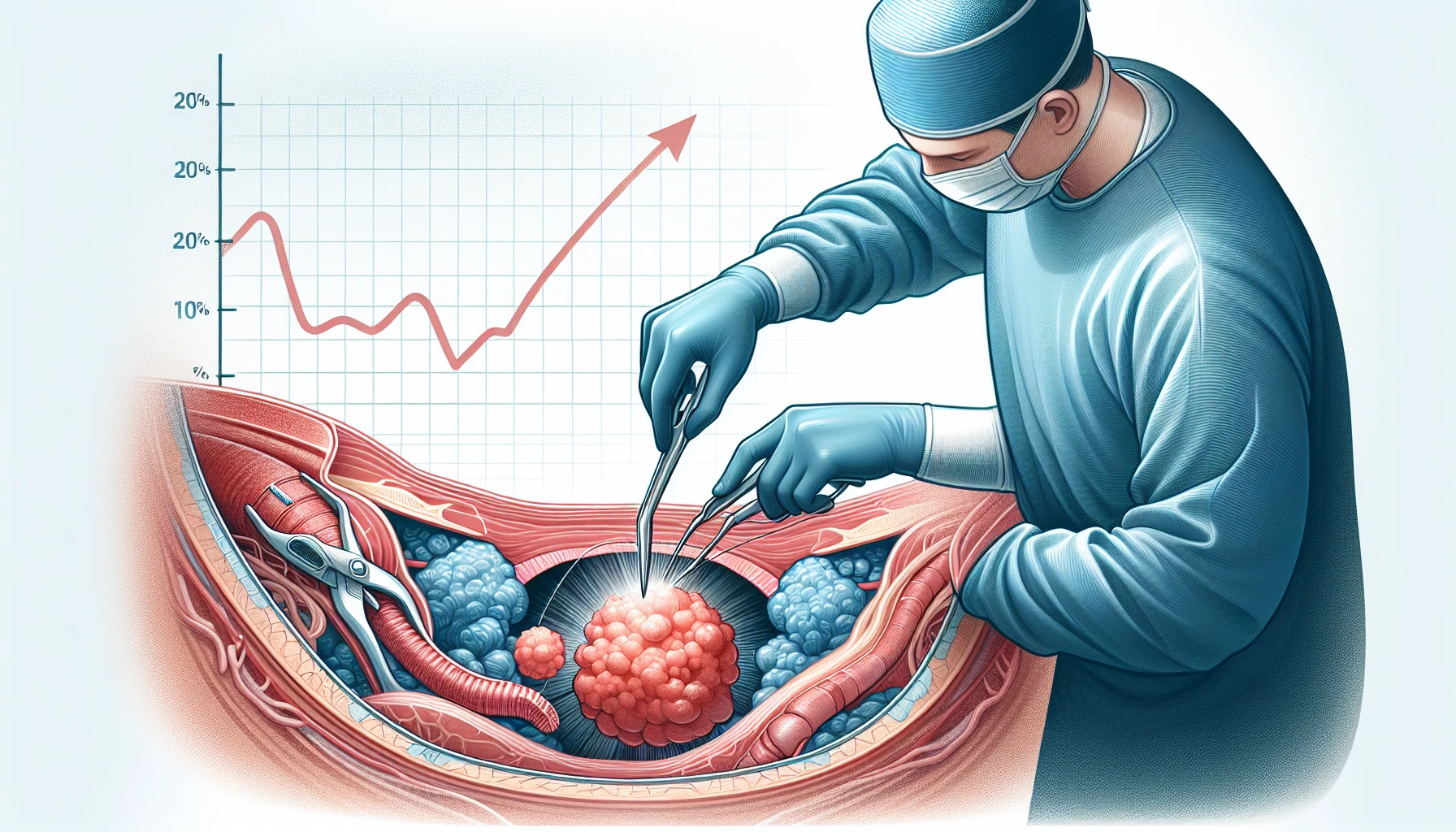
Cytoreductive Surgery (CRS)
Cytoreductive surgery (CRS) is a comprehensive surgical procedure employed to treat peritoneal metastases (PM) from metastatic colon cancer. The goal of CRS is to remove as much tumor tissue as possible, thereby reducing the size of the tumor and improving survival rates in selected patients. Achieving complete cytoreduction is essential for the prognosis of CPM patients.
CRS has demonstrated significant benefits for patients with metastatic colon cancer in the peritoneal cavity, particularly when achieving complete cytoreduction (CCR of zero or one). Furthermore, CRS combined with hyperthermic intraperitoneal chemotherapy (HIPEC) has been effective in treating peritoneal metastases from colorectal cancer.
Nonetheless, CRS is associated with its own set of risks and complications. These may include morbidity and mortality rates, gastrointestinal complications such as intra-peritoneal abscesses, pancreatic fistulas, biliary fistulas, chyle leak, prolonged ileus, and gastric stasis. Careful patient selection and personalized approaches are essential to optimize outcomes in CRS.
Hyperthermic Intraperitoneal Chemotherapy (HIPEC)

Hyperthermic intraperitoneal chemotherapy (HIPEC) involves administering chemotherapy that has been heated, directly into the peritoneal cavity. The benefits of HIPEC include:
-
Improved treatment effectiveness by directly targeting peritoneal metastases
-
Minimized damage to healthy tissues
-
Enhanced patient outcomes and survival when combined with CRS (cytoreductive surgery)
Several considerations must be made when administering HIPEC, such as:
-
Method
-
Duration
-
Temperature
-
Selection of chemotherapeutic agent
-
Carrier solution
-
Timing
The current regimen of choice for HIPEC is oxaliplatin. However, the PRODIGE-7 trial showed no survival benefit of HIPEC in combination with CRS, raising questions about the role of HIPEC in treating peritoneal metastases.
It is worth noting that the results of the PRODIGE-7 trial could be attributed to the fact that 80% of the patients included underwent extensive neo-adjuvant systemic treatment, potentially leading to oxaliplatin-resistance of peritoneal cancer cells, and consequently diminishing the effect of intraperitoneal oxaliplatin. Further research is needed to optimize HIPEC treatment and better understand its role in treating peritoneal metastases.
Systemic Chemotherapy
Adjuvant systemic chemotherapy is an essential component in the treatment of metastatic colon cancer in the peritoneal cavity. It is often used in combination with other treatments, such as CRS and HIPEC, as both neoadjuvant and adjuvant therapy. Systemic chemotherapy is effective in treating inoperable disease and is considered the primary treatment for stage IV colorectal cancer patients.
However, the efficacy of systemic chemotherapy in treating peritoneal metastases is limited due to issues such as the restricted penetration of chemotherapy into the peritoneum and the low tumor-targeting specificity of systemic therapy. Further research is needed to improve the efficacy of systemic therapy in treating peritoneal metastases and to identify patients who may benefit most from this approach.
Clinical Trials and Advancements in Treatment
Recent clinical trials have investigated new treatment options and contributed useful knowledge about the effectiveness of existing treatments like HIPEC. The PRODIGE-7 trial, Pressurized Intraperitoneal Aerosol Chemotherapy (PIPAC), and immunotherapy are just a few examples of advancements in treatment options for patients with metastatic colon cancer in the peritoneal cavity.
PRODIGE-7 Trial
The PRODIGE-7 trial was a phase 3 multicenter study conducted to compare the effects of CRS plus oxaliplatin-based HIPEC versus CRS alone on patients diagnosed with peritoneal carcinomatosis originating from colorectal cancer. The trial was randomized and open-label. The trial results showed that HIPEC combined with CRS had no additional survival benefit when compared to CRS alone. The median overall survival was 41.7 months. 41.2 months; hazard ratio [HR] 1.00 [95% CI 0.63–1.58]). The lack of survival benefit raised questions about the role of HIPEC in treating peritoneal metastases.
The results of the PRODIGE-7 trial could be attributed to the fact that 80% of the patients included underwent extensive neo-adjuvant systemic treatment, potentially leading to oxaliplatin-resistance of peritoneal cancer cells, and consequently diminishing the effect of intraperitoneal oxaliplatin. Further research is needed to optimize HIPEC treatment and better understand its role in treating peritoneal metastases.
Pressurized Intraperitoneal Aerosol Chemotherapy (PIPAC)
Pressurized Intraperitoneal Aerosol Chemotherapy (PIPAC) is a novel treatment option that holds promise for reducing complications and expanding eligibility for CRS and HIPEC. PIPAC involves the administration of oxaliplatin aerosolized in the peritoneal cavity, ensuring a homogeneous distribution throughout the cavity.
By offering a more targeted approach and potentially fewer side effects, PIPAC may increase the number of CPM patients who may be eligible for a curative approach through CRS and HIPEC.
Immunotherapy
Immunotherapy is an emerging treatment option for metastatic colon cancer, with ongoing research exploring its potential benefits in the peritoneal cavity. Immunotherapy, particularly immune checkpoint inhibitor (ICI) therapy, has demonstrated potential in treating metastatic colon cancer in the peritoneal cavity. Recent studies have revealed that ICI therapy can significantly enhance survival in certain types of metastatic colorectal cancer, including those with microsatellite instability (MSI) or deficient mismatch repair (dMMR).
Further research is being conducted to identify additional synergistic mechanisms for disease control through immunotherapy and to evaluate its potential role in treating patients with peritoneal metastases from colorectal cancer. The ongoing investigation of immunotherapy may lead to the development of novel, effective treatments for metastatic colon cancer in the peritoneal cavity.
Prognostic Factors and Survival Rates
Several factors can impact survival rates and treatment outcomes in patients with peritoneal metastases. These include the Peritoneal Cancer Index (PCI), Consensus Molecular Subtypes (CMS), and RAF/RAS mutations.
Comprehending these prognostic factors can assist in guiding treatment decisions and tracking treatment response in patients with metastatic colon cancer in the peritoneal cavity.
Peritoneal Cancer Index (PCI)
The Peritoneal Cancer Index (PCI) is a numerical score used to evaluate the degree of tumor growth in peritoneal metastasis. It divides the abdomen into nine sectors and the small bowel into four additional sectors, resulting in a total PCI score that can range from 0 to 39. The PCI is employed to ascertain the prognosis and operability of peritoneal metastasis.
The PCI score is closely related to overall survival, but it can be difficult to assess preoperatively. Nevertheless, the PCI remains a valuable tool in determining the extent of peritoneal disease and guiding treatment decisions for patients with peritoneal metastases.
Consensus Molecular Subtypes (CMS)
The Consensus Molecular Subtypes (CMS) classification system can help predict survival and treatment response in patients with peritoneal metastases. The CMS classification results in four consensus molecular subtypes (CMS).
Notably, CMS-4 has the worst outcomes and limited response to systemic therapy. Understanding the molecular profile of a patient’s tumor can help guide treatment decisions and optimize outcomes.
RAF/RAS Mutations
RAF/RAS mutations in colorectal cancer are associated with poor prognosis and may impact the effectiveness of certain treatments. These mutations act as downstream messengers of the epidermal growth factor receptor pathway (EGFR), which regulates cell proliferation and survival.
Identifying the presence of RAF/RAS mutations in patients with peritoneal metastases may help guide treatment decisions and monitor treatment response.
Personalized Treatment Approaches
Personalized treatment strategies, including patient selection, targeted therapy, and biomarkers, can enhance treatment outcomes for patients with peritoneal metastases. By tailoring the treatment to the individual patient, it is possible to maximize the chances of tumor control and optimize outcomes.
Patient Selection
Careful patient selection is crucial for maximizing the benefits of treatments like CRS and HIPEC. Factors such as:
-
Presence of peritoneal metastases
-
Absence of liver metastases
-
Prior treatment with neo-adjuvant therapy
-
Patient’s presentation and grade (e.g., presence of signet ring, mucinous)
are taken into account when selecting patients for CRS and HIPEC treatment.
By identifying the most suitable candidates for these treatments, it is possible to enhance the overall success of the treatment approach.
Targeted Therapy
Targeted therapies, such as those targeting RAF/RAS mutations, may improve treatment outcomes for patients with specific molecular profiles. By inhibiting the activity of these molecules, targeted therapies can slow down or halt the growth of cancer cells. Examples of targeted therapy drugs for metastatic colon cancer include BRAF inhibitors such as Encorafenib.
Further research is needed to identify additional targeted therapies and evaluate their efficacy in treating peritoneal metastases.
Biomarkers and Circulating Tumor DNA
Biomarkers, circulating tumor DNA (ctDNA), and tumor cells can help guide treatment decisions and monitor treatment response in patients with peritoneal metastases. By detecting specific mutations, such as RAS mutations, and evaluating the effectiveness of treatment, ctDNA analysis can significantly impact treatment decisions for metastatic colon cancer in the peritoneal cavity.
It is essential to consider the limitations of ctDNA-based treatment decisions and factor in other elements in the overall treatment plan.
Quality of Life and Palliative Care
Improving quality of life and providing palliative care is crucial for patients with metastatic colon cancer in the peritoneal cavity. Pain management, nutritional support, and psychological support can all play a vital role in helping patients cope with the emotional and physical challenges of living with metastatic colon cancer in the peritoneal cavity.
Pain Management
Efficient pain management is key to enhancing the quality of life for patients with peritoneal metastases. Typical pain management techniques for patients with metastatic colon cancer involve:
-
the use of over-the-counter analgesics
-
non-opioid medications
-
behavioral pain management approaches
-
treating the underlying cause
By addressing pain effectively, patients can experience improved comfort and well-being.
Nutritional Support
Nutritional support can aid patients in maintaining their strength and overall health during the treatment for metastatic colon cancer. Some dietary recommendations for patients with metastatic colon cancer in the peritoneal cavity include:
-
Consuming a diet abundant in fruits, vegetables, whole grains, and legumes
-
Maintaining a healthy weight
-
Adhering to a healthful dietary pattern
-
Avoiding red and processed meats
These recommendations offer potential benefits for metastatic colorectal cancer patients with metastatic colon cancer.
Psychological Support
Psychological support, encompassing counseling and support groups, can assist patients in coping with the emotional challenges of living with metastatic colon cancer in the peritoneal cavity. By providing emotional and mental support, psychological interventions can assist patients in managing the challenges and stress associated with their diagnosis and treatment.
In addition, psychological support can create a safe environment for patients to openly express their fears, concerns, and emotions, and assist them in developing coping strategies to improve their overall well-being.
Summary
In conclusion, the challenges and advances in treating metastatic colon cancer in the peritoneal cavity are complex and multifaceted. By understanding the metastatic process, exploring the latest clinical trials, and embracing personalized treatment approaches, we can make strides in improving treatment outcomes and enhancing patients’ quality of life. With continued research and advancements, there is hope for a brighter future for those battling metastatic colon cancer in the peritoneal cavity.
Frequently Asked Questions
What is the prognosis for metastatic colon cancer to the peritoneum?
Although historically the prognosis for metastatic colon cancer to the peritoneum has been poor, with advances in chemotherapy and multiple lines of therapy, there is now a median survival of approximately 2 years and a 5-year survival rate of greater than 20%.
What happens when cancer spreads to the peritoneum?
When cancer spreads to the peritoneum, it often produces fluid in the abdomen called ascites causing abdominal distension and blockage of the intestines. Additionally, it may cause blockage of the kidney ureters leading to hydronephrosis.
How do you treat peritoneal metastases from colorectal cancer?
For treatment of peritoneal metastases from colorectal cancer, therapeutic cytoreductive surgery (CRS), systemic chemotherapy and intraperitoneal heated chemotherapy (HIPEC) may be used. Optimal management should be discussed with a multidisciplinary care team to decide the best approach.
What is the role of cytoreductive surgery (CRS) in treating metastatic colon cancer in the peritoneal cavity?
Cytoreductive surgery (CRS) is an important treatment for metastatic colon cancer in the peritoneal cavity, involving the removal of all visible disease in the area. This comprehensive surgical procedure can significantly reduce PM and improve patient outcomes.
How does hyperthermic intraperitoneal chemotherapy (HIPEC) work in treating metastatic colon cancer?
Hyperthermic intraperitoneal chemotherapy (HIPEC) works to treat metastatic colon cancer by administering heated chemotherapy directly into the peritoneal cavity, which increases effectiveness by targeting the metastases and protecting healthy tissues.






Limited Edition
Top 10
Anti-Cancer Juices & Smoothies
Sign up to get access