Imagine being able to predict your risk of developing genetic colon cancer based on your genetics and family history. This is not a far-fetched concept but a reality in our modern medical landscape. The key to this predictive power lies in understanding the genetics behind colon cancer, a disease that claims hundreds of thousands of lives globally every year. The importance of grasping the intricate relationship between genetics, family history, and genetic colon cancer cannot be overstated. By doing so, we can unlock a new era of preventive medicine and early detection.
Key Takeaways
Decoding the Genetics Behind Colon Cancer reveals inherited syndromes like Lynch Syndrome and FAP that increase colorectal cancer risk.
Identifying hereditary colon cancer requires family history analysis, genetic testing, and mutation-specific screening.
Recent innovations in genetic testing have led to improved strategies for managing colorectal cancer & preventive measures.
Decoding the Genetics Behind Colon Cancer
Our genes are the blueprint of our bodies, and any alterations can have significant implications for our health. Genetics play an integral role in colorectal cancer, with certain inherited syndromes notably escalating the risk of disease development. Inherited syndromes such as Lynch Syndrome and Familial Adenomatous Polyposis (FAP) contribute to a significant percentage of all colorectal cancer cases.
Inheriting a cancer syndrome not only elevates the individual’s risk but also represents a considerable risk for first-degree relatives who may inherit the syndrome. This highlights the significance of genetic testing, a tool endorsed by the National Cancer Institute, to identify individuals at risk and shape screening and prevention methods. Comprehending the genetic factors contributing to nearly 30% of all colorectal cancer cases allows for better direction of diagnostic and therapeutic interventions, helping manage elements that escalate colorectal cancer risk.
Lynch Syndrome: The Most Common Inherited Syndrome
Lynch Syndrome is a prevalent inherited colon cancer syndrome caused by a mutation in DNA mismatch repair genes. It is linked to a higher likelihood of developing:
Colorectal cancer
Endometrial cancer
Stomach cancer
Brain cancer
Individuals with Lynch Syndrome are at a considerably elevated lifetime risk of developing colorectal cancer, with estimates as high as 50-80%.
Identifying Lynch Syndrome is a systematic process that includes genetic testing when personal and/or family history criteria are met. Diagnostic tools include analyses of a patient’s family history, tumor testing, and the Revised Bethesda Guidelines for colon or rectal cancer.
Familial Adenomatous Polyposis (FAP) and Its Variants
Familial Adenomatous Polyposis (FAP) is another severe condition resulting from germline mutations in the APC gene, leading to the formation of numerous colonic adenomas and a heightened susceptibility to develop colorectal cancer. The location of the mutation within the APC gene correlates with the severity of colonic polyposis, which can have implications for the clinical management of the disease.
Individuals with FAP face an almost 100% risk of developing colorectal cancer if left untreated, usually diagnosed around the average age of 39 years. Variants such as attenuated FAP pose a lower, yet still substantial lifetime risk, with an average of 69%.
Other Genes Implicated in Hereditary Colon Cancer
Beyond these well-known syndromes, other genes such as MUTYH are implicated in hereditary colon cancer. MUTYH-Associated Polyposis (MAP) is a genetic condition resulting from mutations in the MUTYH gene. The colonic characteristics of MAP can be likened to those of attenuated Familial Adenomatous Polyposis (FAP). The MUTYH gene product plays a crucial role in the base-excision repair pathway, essential for defending against oxidative DNA damage and preventing mutations that could potentially lead to cancer.
MAP follows a recessive inheritance pattern, meaning that siblings of individuals with biallelic MUTYH mutations have a 25% chance of also having MAP. Genetic testing for MAP is conducted by targeting the specific ethnic allelic frequencies of MUTYH variants, highlighting the importance of considering the ethnic background during testing.
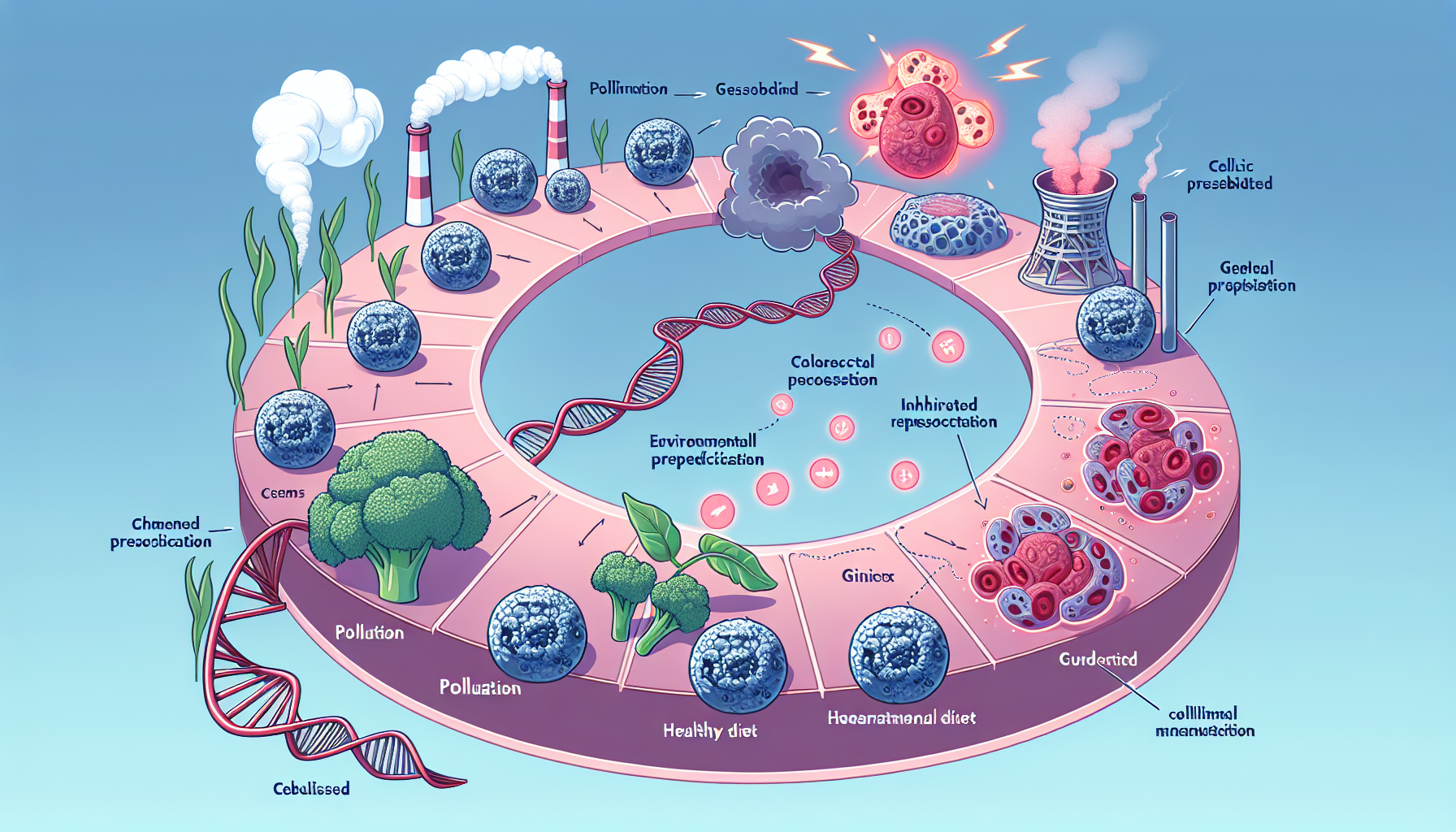
The Spectrum of Colorectal Cancers: From Hereditary to Sporadic
Although hereditary forms of colorectal cancer present a significant risk, it’s worth mentioning that the majority of colorectal cancer cases, about 90%, are sporadic. In the United States, approximately 1 in 23 individuals will develop sporadic colorectal cancer. Age is a critical factor in colorectal cancer risk, with the likelihood of developing the disease increasing after the age of 50.
Sporadic colorectal cancer development is primarily influenced by the accumulation of somatic genetic and epigenetic events, coupled with lifestyle factors like a Western diet, smoking, obesity, diabetes, alcohol consumption, and exposure to carcinogens. Grasping the entire spectrum of colorectal cancers, from hereditary to sporadic, is key for customizing prevention and treatment strategies.
Identifying Hereditary Colorectal Cancer
The detection of hereditary colorectal cancer requires a comprehensive approach, encompassing family history analysis, genetic testing, and mutation-specific screening. Specific gene mutations linked to hereditary colorectal cancer include mutations in the APC, DCC/MADH2/MADH4, TP53, MLH1, MSH2, MSH6, and PMS2 genes.
Family history has a pivotal role in detecting hereditary colorectal cancer, including hereditary nonpolyposis colorectal cancer, by evaluating if close relatives had the disease. A pattern of colorectal cancer across multiple family members can indicate a hereditary syndrome or genetic factors at play, guiding healthcare professionals in deciding if more genetic testing and screening is needed.
Initial indications of hereditary colorectal cancer may encompass persistent alterations in bowel habits, blood in the stool, abdominal pain or cramping, unexplained weight loss, and fatigue.
Sporadic Colon Cancer: Environmental and Age-Related Factors
Being the more prevalent type, sporadic colon cancer represents the majority of colorectal cancer instances. Lifestyle factors play a significant role in its development, with dietary factors like high red and processed meat intake, low vegetable and fruit intake, and high alcohol consumption linked to an increased risk. Obesity and physical inactivity also significantly heighten the risk of developing colorectal cancer.
Both smoking and excessive alcohol consumption have been shown to elevate the risk of developing and succumbing to colorectal cancer. Chronic alcohol consumption is linked to the formation of colorectal polyps and the onset of colon cancer.
Screening and Prevention Strategies for High-Risk Individuals
For those at high risk of developing colorectal cancer, personalized screening and prevention strategies are paramount. Those with a significant family history or a first-degree relative diagnosed with colorectal cancer before the age of 60 should consider genetic testing and screening at an earlier stage than the general population.
Colorectal cancer screening recommendations:
Screening should be initiated at an age 10 years younger than the youngest age of diagnosis in the family, or at age 40, whichever is younger.
Screening should be repeated every five years.
Regular colonoscopy every 1-2 years is advised for high-risk individuals, starting by the age of 20-25 years.
If colorectal cancer is found, subtotal colectomy with ileorectal anastomosis is recommended.
Annual rectal surveillance should be conducted after surgery.
When to Begin Colorectal Cancer Screening
The commencement of screening for colorectal cancer relies on individual risk factors. For the general population without a family history or inherited gene mutations, screenings should commence at the age of 45. However, for those with a family history of the disease, screenings should begin earlier.
If one first-degree relative was diagnosed with colorectal cancer before the age of 60, or two at any age, individuals should begin screening at age 40. Alternatively, they should start screening 10 years earlier than the earliest diagnosis in their family, whichever comes first..
If a first-degree relative has had colorectal cancer or a documented advanced adenoma, it is recommended to start screening at age 40, or 10 years before the youngest age at which the relative was diagnosed. This helps in early detection and preventive measures..
For those diagnosed with Lynch Syndrome, a colonoscopy is advised every 1 to 2 years.
Surveillance Techniques for Early Detection
Surveillance techniques for the early detection of hereditary colorectal cancer include:
Colonoscopy
Genetic testing
High-sensitivity fecal occult blood testing
Flexible sigmoidoscopy
Endoscopy
These methods play a vital role in detecting colorectal cancer at an early stage.
Colonoscopy, despite its invasive nature and potential risks, is the preferred method for detection because it allows for the removal of polyps during the procedure. Meanwhile, genetic testing provides insights into inherited changes in a person’s genes, uncovering diseases, identifying potential risks, and informing medical interventions to reduce disease risk. Together, these techniques provide a comprehensive approach to early detection, with impressive diagnostic accuracy rates.
The Importance of Family Health History in Assessing Cancer Risk
Comprehending your family health history is vital in evaluating your risk for developing colorectal cancer. It reveals patterns of disease and conditions that may run in your family and helps in identifying more individuals who might be at high risk. A comprehensive family health profile should include information about:
Relatives who have had cancer
Ages at diagnosis
Types of cancer
Any known genetic mutations or syndromes
Other relevant medical history, such as chronic diseases or conditions in the family
Comprehending your family history is key to the prevention of colorectal cancer. Individuals with a first-degree relative who has had colon cancer are deemed to be at high risk for developing colorectal cancer themselves. Moreover, patient evaluations to aid in the detection and identification of family cancer syndromes may include:
Genetic counseling
Formal genetic testing
Colonoscopy
Regular follow-up exams
Referrals to other medical specialists as needed
Building a Comprehensive Family Health Profile
Building a comprehensive family health profile entails:
Gathering health information about oneself and immediate family members
Acquiring detailed records of family members’ health conditions and medical histories
Noting any genetic disorders or hereditary conditions within the family
Documenting the age and cause of death of family members
Recording lifestyle factors like smoking, alcohol consumption, and exercise habits of family members.
The number of affected relatives can significantly influence the accuracy of a family health profile. Here are some key points to consider:
A larger number of affected relatives suggests a higher likelihood of hereditary conditions.
It also indicates an increased risk for other family members.
Having more affected relatives can help healthcare professionals make more accurate diagnoses and treatment plans.
Genetic testing complements the family health profile by offering insights into:
Inherited changes in a person’s genes
Uncovering diseases
Identifying potential risks
Informing medical interventions to reduce disease risk.
Genetic Counseling: A Crucial Step for At-Risk Families
Genetic counseling is a pivotal step for families at risk of hereditary colorectal cancer. It involves:
Using genetic tests to determine whether individuals from specific families have inherited a heightened risk of developing colorectal cancer due to inherited cancer syndromes.
Reviewing the patient’s family history and determining if genetic testing is necessary.
Providing guidance and support in understanding the risks and implications of genetic factors related to colorectal cancer.
Identifying inherited cancer syndromes such as Lynch syndrome or familial adenomatous polyposis.
Genetic counselors play a crucial role in this process.
Genetic counseling is recommended for individuals with:
a personal or family history of colon cancer
other types of cancer
multiple family members affected by colorectal cancer
colorectal cancer at a young age, typically 35 years or younger
The process entails a genetic counselor carefully examining the patient’s family history and ascertaining the need for genetic testing.
Managing Life with a Hereditary Cancer Syndrome
Coping with a hereditary cancer syndrome necessitates certain lifestyle adjustments and use of support systems to reduce cancer risk and maintain overall health. Individuals with a hereditary cancer syndrome should consider:
Maintaining a healthy weight
Engaging in regular physical activity
Following a healthy diet
Avoiding smoking
Stress management also plays a crucial role in mitigating the risk of hereditary cancers by reducing psychological distress and enhancing the quality of life for affected individuals.
Helpful support resources for individuals dealing with hereditary cancer syndromes encompass robust family support and participation in research initiatives focused on recognizing and addressing the needs of individuals with inherited cancer syndromes.
Lifestyle Adjustments to Mitigate Cancer Risk
Certain lifestyle modifications are advised to reduce the risk of colorectal cancer. Some of these modifications include:
Maintaining a healthy weight, as compelling evidence indicates a protective impact against the disease
Consuming oatmeal, yogurt, citrus fruits, bell peppers, fish, broccoli, cabbage, and vitamin-C rich fruits like oranges
Reducing the consumption of a Western diet high in processed foods and unhealthy fats
Adopting these changes can help lower the risk of colorectal cancer, as opposed to certain lifestyle factors that may increase colorectal cancer risk.
Beyond dietary adjustments, regular physical activity is advantageous in diminishing the risk of colon cancer. By complementing dietary modifications as part of a holistic approach to mitigate the risk, regular workouts can significantly lower the risk of developing colorectal cancer.
Support Systems and Resources
When coping with a hereditary cancer syndrome, the importance of a robust support system is undeniable. Patient advocacy groups like Facing Our Risk of Cancer Empowered (FORCE) offer support, education, and resources for individuals and families affected by hereditary cancer syndromes. Support groups offer individuals with hereditary cancer syndromes valuable information, emotional support, and a sense of community. They enable individuals to connect with others facing similar experiences, share concerns and fears, and gain insights from others’ experiences.
Online resources accessible to individuals affected by hereditary cancer syndromes include:
Facing Our Risk
UCSF BRCA Program
The Jackson Laboratory
Cancer.Net
MSK CATCH
These resources offer information, support, and access to healthcare experts and services for individuals affected by hereditary cancer syndromes. Online forums can offer significant benefits for those living with hereditary cancer syndromes, serving as a platform for individuals to connect with others facing similar experiences, exchange valuable information, and provide mutual support.
Innovations in Genetic Testing and Research
There have been notable advancements in genetic testing and research related to colorectal cancer in recent years. For instance, the FDA authorization of the Invitae Common Hereditary Cancers Panel enables the detection of inherited genetic changes that elevate the risk of colon cancer. Additionally, the FDA has approved blood tests for identifying inherited genetic changes linked to an increased risk of hereditary colon cancer.
Tumor testing has a vital role in personalized medicine, providing insights into the specific genetic mutations and biomarkers present in the tumor. This data aids in customizing treatment plans to address the unique characteristics of the tumor, thereby offering more effective and personalized treatment options for patients.
Significant progress has been made in the study of gene mutations and their impact on colon cancer, including:
The identification of a new gene crucial to the growth of colon cancer
Progress in NCI-funded research for prevention, detection, and treatment
The revelation of a mechanism enabling gene mutations to aid tumors in evading detection
Comprehensive studies unveiling new genetic risk factors.
The Role of Tumor Testing in Personalized Medicine
Tumor testing is a critical component of personalized medicine. It involves the thorough analysis of the genetic and molecular characteristics of a tumor to inform personalized treatment decisions for individual patients. By identifying specific mutations or biomarkers in the tumor, oncologists can determine the most suitable treatment options for each patient.
Tumor testing, including multi-gene panel sequencing and biomarker testing, identifies genetic alterations and biomarkers instrumental in determining the distinct attributes of a colon cancer tumor. This data is essential for tailoring treatment plans for colon cancer patients, enabling healthcare providers to choose the most suitable therapies and personalized treatment options according to the tumor’s individual genetic profile.
Emerging Research on Gene Mutations and Cancer Risk
Emerging research continues to illuminate the complex relationship between gene mutations and cancer risk, greatly enhancing our understanding and leading to evolved strategies in managing colorectal cancer. Through whole-genome sequencing, new insights into germline mutations in the POLE and POLD1 genes have been uncovered, contributing to the understanding of a novel form of the disease. Additionally, the identification of crucial genes associated with colon cancer growth represents a noteworthy progress.
Recent research also plays a crucial role in the development of preventive measures for colon cancer. Studies indicating the potential of aspirin to activate protective genes and slow down the progression of colon cancer are highly impactful. Additionally, this research is essential for the discovery of new screening tests, diagnostic techniques, and medications that aid in early detection and prevention.
Summary
In summary, understanding the genetics behind colorectal cancer and the role of family history in assessing risks is a critical step towards effective prevention, early detection, and personalized treatment strategies. From inherited syndromes like Lynch Syndrome and Familial Adenomatous Polyposis to sporadic colorectal cancer, it is clear that both genetic and lifestyle factors play significant roles in colorectal cancer risk.
Early and tailored screening, lifestyle adjustments, and the utilization of support systems are all crucial components in managing life with a hereditary cancer syndrome. As our understanding of gene mutations and cancer risk continues to expand through innovative research and advancements in genetic testing, we are moving closer to a future where colorectal cancer can be effectively prevented, detected early, and managed effectively.
Frequently Asked Questions
What type of colon cancer is hereditary?
Approximately 5 to 10 percent of colon cancer is hereditary, with Lynch Syndrome (previously known as Hereditary Non-Polyposis Colorectal Cancer or HNPCC) and Familial Adenomatous Polyposis (FAP) being the major hereditary colon cancer syndromes.
What is the life expectancy for Lynch syndrome?
People with Lynch syndrome may experience a normal life expectancy with appropriate monitoring and management of their cancer risk, but it can vary depending on their specific genetic mutations and the type and stage of cancer they develop. Ten-year overall survival is estimated to be 80.5%, and fifteen-year overall survival is estimated to be 70%.
Is Lynch syndrome passed from mother or father?
Lynch syndrome is inherited in an autosomal dominant pattern, meaning that a gene mutation needs to happen in only one copy of the gene to increase the risk of getting the disease. Both parents can pass on this gene mutation, and the chance of inheritance is 50%.
What lifestyle adjustments can be made to mitigate the risk of colorectal cancer?
To reduce the risk of colorectal cancer, maintain a healthy weight, engage in regular physical activity, follow a healthy diet, and avoid smoking.
What are the recent advancements in genetic testing and research for colorectal cancer?
Recent advancements in genetic testing and research for colorectal cancer include the FDA authorization of the Invitae Common Hereditary Cancers Panel, the approval of blood tests for identifying inherited genetic changes linked to an increased risk of hereditary colon cancer, and the use of tumor testing as a tool for personalized medicine.






Limited Edition
Top 10
Anti-Cancer Juices & Smoothies
Sign up to get access